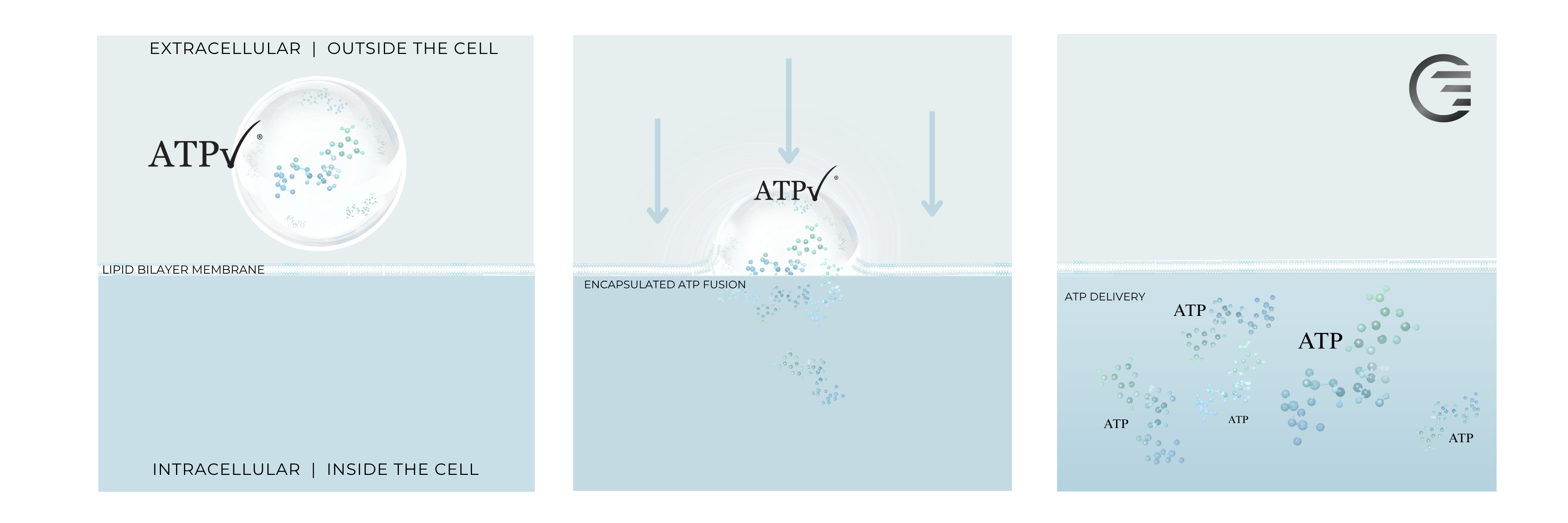
Lipid vesicle-cell membrane fusion offers an attractive means for delivery of substances to cells.
Unlike endocytosis, which takes minutes for the process of internalization of lipid vesicles, membrane fusion occurs on the seconds scale. This equates to a higher delivery rate of encapsulated substances, and furthermore, the delivery of the substance to the cytoplasm, compared to trafficking of endocytotic vesicles for lysosomal processing. For substances like ATP that are consumed rapidly by cells, membrane fusion offers a method of delivery that is significantly faster than using endocytosis.
Furthermore, lipid vesicle-cell membrane fusion has been recently shown by Moderna and Pfizer as an efficient means of delivery of polynucleotides (RNA) to human cells. Lipid vesicles also protect the encapsulated substances from rapid enzymatic degradation (from ectonucleotidases for example), which also adds to the efficiency of substance delivery offered by membrane fusion.
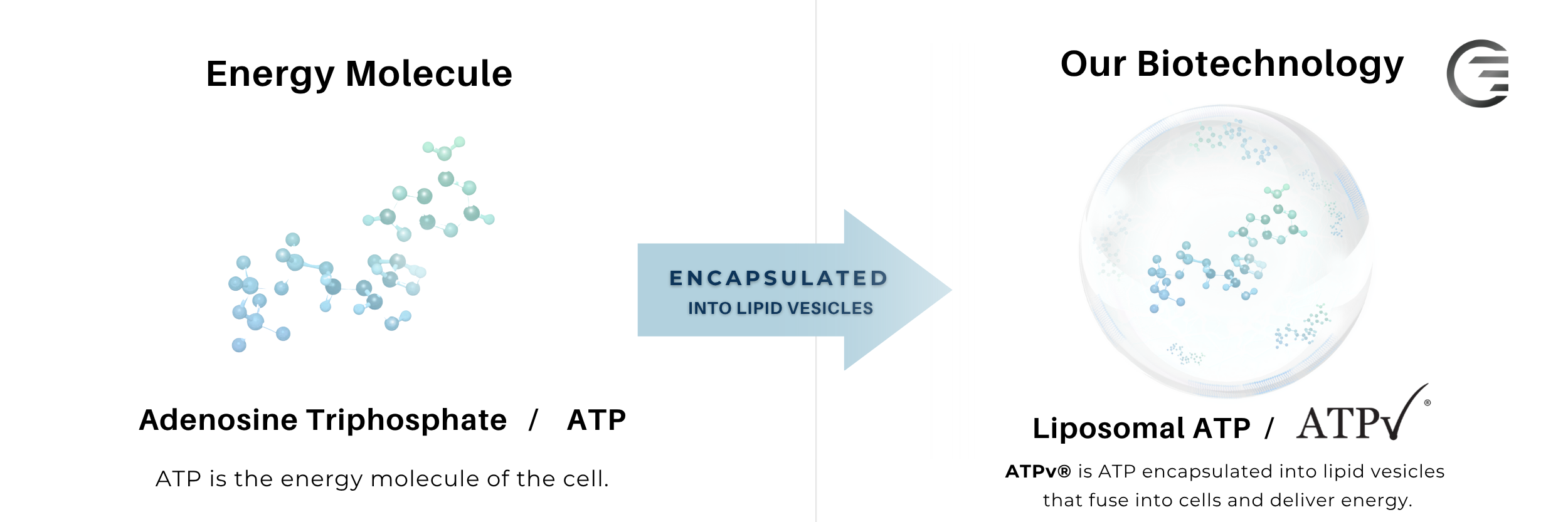
Adenosine Triphosphate (or ATP) is a molecule that is made naturally in the body. ATP is
used as an energy source or signaling molecule and is crucial for proper cellular function, wound healing and repair, formation of DNA and proteins, and a myriad of other functions. Simply put, without enough ATP your cells would die.
Our patented liposomal ATP formulation is called ATPv (shortened for ATP in vesicles). Here we have utilized lipids to form a liposome (or lipid vesicle) and have encapsulated the ATP molecule inside. Our unique formula allows for rapid fusion and delivery of ATP to cells, boosting the available ATP for cellular functions.

The Future of Our Technology
The possibilities of Liposomal ATP Technology are far reaching and could be the solution for needs in medicine.
- Wound Healing
- Hair Restoration
- Cosmetic Skincare
- Hemorrhagic Shock
- Organ Preservation
- Limb Transplantation
- Cell & Tissue Preservation
Technology Avenues of ATPv®

SKIN | ATP
Adenosine-5’-triphosphate (ATP) is the universal energy currency of all living organisms. ATP plays a role in every process associated with living organisms, as it is required for the production and use of proteins, lipids, carbohydrates, and nucleic acids. In human skin, ATP plays a central role in cell proliferation, cell integrity, cell signaling, production of trophic factors, maintenance of the extracellular matrix, oxygen radical formation and reduction, and maintenance of the transdermal barrier.
Learn more at SKINATP.com
Tissue Preservation
There are four types of tissues in the human body: Connective, Epithelial, Muscle, and Nervous tissues. Each of these tissues are composed of cells that provide the structure and function of the tissue. When more than one of these tissues are combined it is called a composite tissue. Examples of composite tissues include, skin, bone, and eyes, and teeth to name a few. As the size of the composite tissue increases, the complexity of preserving the tissue also increases. It is easier to preserve a piece of skin than it is to preserve a severed leg. This is illustrated by the surgical success of reattaching severed skin compared to reattaching a severed limb, in which the former can last for 6-10 hours in preservation while the latter can last for 1-2 hours.
The cells that compose tissues require a constant supply of blood in order to receive nutrients and oxygen in order to function and remain alive. When a tissue loses blood flow, or when blood flow is decreased, the loss of nutrients and oxygen results in a decrease in cell ATP. Cells can conserve ATP during periods of low blood flow by shutting down certain ATP consuming processes, and cells can make ATP without oxygen (glycolysis), but these survival mechanisms only last for a short period of time. Furthermore, as the tissue becomes larger and more complex, the higher the demand for ATP, and the more difficult it is to preserve cells that are deeper within the tissue.
ATP is a water-soluble molecule that does not pass-through cell membranes, and does not last long outside of cells. Thus providing ATP alone to tissues is not an effective means of tissue preservation. To get ATP to the cells of a tissue requires a vector that can make the molecule capable of crossing cell membranes, and protecting it from degradation. In large composite tissues, such as a severed leg, it is difficult to provide ATP to cells deep within the tissue space. However, the most important cells that must be preserved in a composite tissue preservation are the cells that line blood vessels, called endothelial cells. Maintaining endothelial cell survival preserves the blood vessels of the tissue and allows the tissue to be connected back to its blood supply. When a composite tissue is perfused with liposomal ATP the endothelial cells are in direct contact with the solution, allowing these cells to survive periods outside of the body. When blood flow is restablished, tissue stem cells can help regenerate certain parts of the tissue that were damaged by the preservation process, but without blood flow, this is impossible.
Hemorrhagic Shock | ATP
Trauma is the leading cause of death for people under 40 years of age, and 80% of these deaths involves severe blood loss. When there is significant blood loss, the body’s blood vessel network shifts blood to areas that are important for life. This means that blood flow to the extremities and other non-vital areas, such as the intestines is decreased. The conservation of blood flow maintains internal organ blood flow and pressure, essential to survival. However, the loss of blood flow to the intestines leads to a large immune response and a shift of fluid from the blood into the tissues. These events lead to a condition called hemorrhagic shock, that will ultimately lead to organs shutting down, and death.
The origin of hemorrhagic shock begins with poor blood flow to the intestines. Without adequate blood flow, the intestinal blood vessels become leaky thus allowing substances associated with the intestines to enter into the blood. The cause of the leaky blood vessels is due to ischemia-reperfusion injury, which is where tissue that was without blood flow is reoxygenated and releases substances harmful to the body. To decrease ischemia-reperfusion injury, the level of ATP in the intestinal blood vessels needs to be increased.
The current gold-standard for treating severe blood loss is to provide whole blood. While this technique can increase blood pressure and volume, it does not address the issue of ischemia-reperfusion injury in the intestines. Using a combination of whole blood that contains liposomal ATP could decrease injury to the intestines, and thus decrease the severity of hemorrhagic shock.
Tissue Preservation
Organs are specialized composite tissues that provide specific function for the body. Each organ has a different demand for ATP, based on its function. For example, the heart has a high ATP demand and can last only a few minutes without blood flow, whereas a kidney has a lower ATP demand and can last for hours without blood flow. This difference in ATP demand suggests that each organ requires a unique approach to preservation outside of the body.
Current organ preservation solutions contain additives that help the cells of the organ produce ATP. This includes substances like glucose, glutamate, adenosine, and oxygen to name a few. These substances do not make ATP directly but require a metabolic pathway to help make ATP. Each metabolic pathway has numerous enzymes that are responsible for helping make ATP using these substrates. Enzyme activity (how fast an enzyme can function) is related to temperature; The colder a solution is the slower the enzymes activity.
This means that the production of ATP is dependent on the temperature of the organ preservation solution. While it is true that as the organ is kept colder the demand for ATP decreases, there is a fine balance between ATP consumption and ATP production, that is often difficult to maintain. This can be due to depletion of the additives (e.g., glucose), or the accumulation of metabolic by-products (CO2, acid, oxygen radicals) that occur when making ATP.
Research shows liposomal ATP allows for the successful delivery of ATP directly to the cells of the organ. It also protects the ATP from degradation until it can be used by the cells of the organ. In addition, since no metabolic pathway was used to make ATP, the production of metabolic by-products is not a factor. In addition, due to the size of the liposome (nanometers), liposomes can pass through gaps between cells or take advantage of fenestrae. This allows the penetration of ATP to cells that are distant from the blood vessel network of the organ.
Our Products
-
ATPv®, 50 mL
Regular price $288.00 USDRegular priceUnit price / per -
ATPv®, 25 mL
Regular price $168.00 USDRegular priceUnit price / per -
Vitalise Wound Care Spray
Regular price $350.00 USDRegular priceUnit price / per -
ATPv®, 6mL
Regular price $63.00 USDRegular priceUnit price / per